Menopause and injury risk: Why injuries increase during menopause and how to recover faster
The menopause is a natural life transition, but many women are surprised by how much it affects their muscles, joints, tendons, and bones. If you’ve noticed new aches, stiffness, tendon pain, or injuries that take longer to heal, you’re not imagining it. Hormonal changes, particularly the decline in oestrogen, significantly affect injury risk and recovery. In this article, we explain:
- Why menopause increases injury risk
- Why recovery can take longer
- The three most common injuries during menopause
- What you can do to stay strong and injury-free
How does the menopause increase injury risk?
During perimenopause and menopause, oestrogen levels decline. Oestrogen is essential for maintaining healthy connective tissue, muscle mass, and bone density. When oestrogen drops, several key changes occur:
1. Reduced collagen production (weaker tendons and ligaments)
Oestrogen helps regulate collagen synthesis. Collagen gives tendons and ligaments their strength and elasticity.
Lower oestrogen can lead to:
- Stiffer, less elastic tendons
- Reduced tendon load tolerance
- Increased risk of tendinopathy
- Higher ligament injury risk
This is why many menopausal women develop persistent tendon pain.
2. Loss of muscle mass and strength
Muscle loss (sarcopenia) accelerates during menopause. Without structured strength training, women can lose 1–2% of muscle mass per year.
Reduced muscle strength means:
- Less shock absorption
- Higher stress is placed on joints
- Increased overload on tendons
- Greater fall risk
Muscles protect joints. When muscle strength declines, injury risk increases.
3. Reduced bone density
Oestrogen plays a critical role in bone turnover. As levels fall:
- Bone resorption increases
- Bone mineral density decreases
- Risk of osteoporosis rises
This increases the risk of:
- Stress fractures
- Spinal compression fractures
- Hip fractures
Women who suddenly increase activity (e.g. starting running or high-intensity classes) are particularly vulnerable.
4. Increased inflammation and pain sensitivity
Lower oestrogen is associated with higher systemic inflammation. This can:
- Increase general joint pain
- Slow healing
- Heighten pain sensitivity
- Cause old injuries to flare up
Sleep disturbances are common during menopause and further reduce recovery capacity.
Why does injury recovery take longer during the menopause?
Many women report that injuries “just don’t heal like they used to.” There are physiological reasons for this.
Slower tissue repair.
Lower oestrogen reduces fibroblast activity (cells responsible for collagen repair).
This can result in:
- Slower tendon healing
- Delayed muscle repair
- Persistent tendinopathy
Reduced strength adaptation.
Hormonal changes may blunt strength adaptations if loading is insufficient. Rehabilitation and strength programmes often require:
- Progressive heavy resistance training
- Longer recovery periods
- Careful load management
Joint stiffness.
Reduced cartilage hydration and lubrication lead to:
- Morning stiffness
- Reduced mobility
- Compensatory movement patterns
Without targeted rehab, this can prolong recovery.
The 3 most common injuries we see in menopausal women are.
1. Gluteal tendinopathy (Lateral Hip Pain)
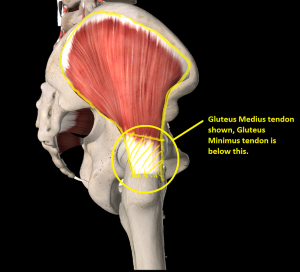
Gluteal tendinopathy, sometimes but incorrectly known as Greater Trochanteric Pain Syndrome (GTPS), is extremely common during the menopause.
Why does this happen?
- Reduced collagen quality
- Weak hip abductors
- Increased tendon stiffness
- Hormonal influence on tendon metabolism
Symptoms to look for.
- Pain on the outside of the hip
- Pain lying on that side
- Discomfort walking uphill or climbing stairs
The treatment for this condition focuses on reducing pain and improving symptoms.
- Progressive hip strengthening
- Load modification
- Avoiding compressive positions early on
2. Plantar fasciitis (Heel pain)

Heel pain is another frequent complaint during menopause.
Why does it develop?
- Reduced tissue elasticity
- Calf weakness
- Changes in foot biomechanics
- Increased body weight redistribution
Symptoms to look for.
- Heel pain with the first steps in the morning
- Pain after prolonged standing
- Tight calves
The treatment for this condition focuses on reducing pain and improving symptoms.
- Calf strengthening
- Plantar fascia loading exercises
- Gradual activity progression
3. Stress Fractures and Osteoporotic Bone Injuries

As bone density declines, bone stress injuries become more common.
Common Sites that these occur are as follows.
- Metatarsals (foot bones)
- Tibia/Fibula
- Spine
- Hip (neck of femur)
Risk factors in developing a stress fracture.
- Rapid increase in exercise
- Low vitamin D
- Low resistance training history
- Undiagnosed osteopenia or osteoporosis
Warning signs to look out for.
- Localised bone pain
- Pain worsens with impact
- Pain that does not settle with rest
These injuries require early assessment to prevent progression.
How to reduce your risk of developing an injury during the menopause.
1. Prioritise strength training
Progressive resistance training is the most effective intervention for:
- Maintaining muscle mass
- Improving tendon capacity
- Increasing bone density
- Reducing joint pain
Focus on multi-joint compound movements such as:
- Squats
- Deadlifts
- Step-ups
- Hip thrusters
- Bench press
- etc
Heavy, controlled loading improves tissue resilience and increases robustness.
2. Manage training load
Avoid sudden increases in:
- Running mileage
- Class/gym frequency
- Intensity
Gradual progression allows tendons and bones to adapt.
3. Optimise nutrition for recovery
Key components:
- 20–30g protein per meal
- Adequate calcium intake
- Vitamin D supplementation (if deficient)
- Omega-3 fats
Good nutrition supports tissue repair and bone health.
4. Improve sleep quality – get yourself a Whoop or similar
Better sleep improves:
- Hormone regulation
- Tissue repair
- Pain sensitivity
- Recovery speed
Address night sweats, caffeine timing, and sleep routine.
5. Consider hormone replacement therapy (HRT)
For some women, HRT may support:
- Bone density maintenance
- Muscle preservation
- Reduced inflammation
- Improved sleep
A GP or menopause specialist can advise on suitability.
Final thoughts: Menopause does not mean fragility!
Menopause increases injury risk and can slow recovery, but it does not mean you must stop being active. With the correct strength programme, appropriate load management, and targeted rehabilitation, women can remain strong, resilient, and pain-free throughout menopause and beyond.
If you are experiencing persistent pain or unexplained bone pain during menopause, early assessment and structured rehabilitation are key to a full recovery.

1 thought on “Menopause and injury risk”
Hi, this is a comment.
To get started with moderating, editing, and deleting comments, please visit the Comments screen in the dashboard.
Commenter avatars come from Gravatar.